Thank you for inviting me here today. I have been asked to speak on my experience as an obstetrician in Ireland; therefore my contribution is based on clinical consideration.
This report does not make easy reading but it highlights the complexity of issues surrounding termination of pregnancy in this country. This subject provokes strong views and many differences of opinion. Somewhere in the midst of personal opinion is the need to ensure that women in Ireland have access to sound clinical care. It is impossible not to be affected by the personal testaments of individual women and their partners and while every case is unique, the stories and experiences described will resonate across Irish society and particularly with the 4,000 women who travel to the UK every year in all kinds of circumstance. It is evident that in the present situation, women will continue to travel to the UK or download unknown pills over the Internet in desperation.
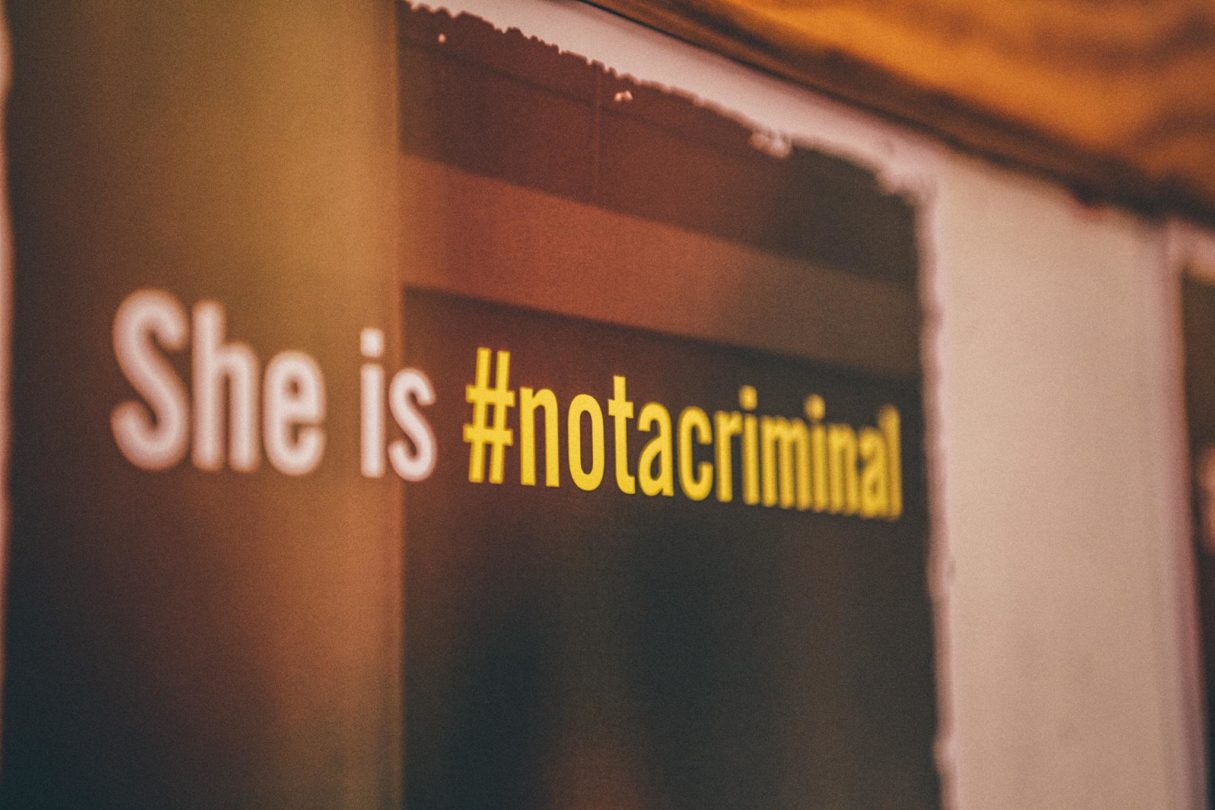
In Ireland a woman qualifies for a termination of pregnancy if there is a real and substantial risk to her life that may be removed only by termination of pregnancy. The process which determines this qualification is cumbersome and complicated and despite the fact that it relies on clinical judgement delivered in good faith to save a woman’s life it is framed in a criminal context. An error in clinical judgement is potentially punishable by a custodial sentence of 14 years for both the mother and her clinician in the event that an identified risk is deemed not substantial enough. Equally, waiting for a woman to be sufficiently ill so that she is perceived to be at risk of dying is potentially dangerous. It relies on a range of presumptions. Firstly, it assumes that we can accurately predict the risk of dying. Haemorrhage, infection, heart disease, liver disease and a host of other disorders can make you very ill but they can also kill you. The point at which serious illness progresses to risk of dying does not come clearly marked. It is not always clinically possible to separate the two nor is it possible to predict clinical course with precision. For example, a young woman with sepsis can appear relatively well despite advanced infection – but she can decompensate suddenly and unpredictably. It is then to be hoped that modern medicine can save her. Performing a medical or surgical procedure in a woman who is already at risk of dying confers additional risk but that is the current requirement of the law. And clinicians are tasked with getting it right in what can be a very narrow window.
I have previously discussed the concept of substantial risk to life and I say it again. What is a substantial risk to life……….Is it 10%, 50%, or 80% risk of dying. This is medical roulette. And what of a woman’s view of the risk presented to her. She must also be part of the negotiation to protect her life. Doctors are no strangers to risk assessment. We frequently counsel patients about a range of risks and potential outcomes. We arrive at a decision with our patients input which we believe is in the best interest of our patient but I cannot think of any other circumstance where risks to life are balanced in the shadow of a custodial sentence for both the clinician and the woman.
Of course in Obstetrics we deal with two lives inextricably linked by a complex physiology. This is dealt with in the Constitution by a balance of rights. The equal right to life of the mother and the fetus. From a medical perspective, this provision it creates difficulty in its presumption that the implications of a range of complex medical disorders can be reduced to a matter of individual right. If the legal world explores the balance of rights, the medical world explores the balance of risk. In a pregnancy complicated by serious disease, clinically it is not a question of right; it is a question of risk. Prior to fetal viability, we do not have the option of delivering a fetus because the fetus cannot survive; therefore, prior to fetal viability this constitutional provision makes no clinical sense. However, its presence facilitates a real possibility that clinical decision-making may be delayed or distorted as clinicians ponder the law rather than medicine.
Unfortunately, there is evidence of this. I will never forget the High Court judgement that dominated last Christmas when somatic function was maintained in a dead woman so that her fetus could be incubated in what could only be described as a macabre experiment. This occurred against a backdrop where the overwhelming clinical judgement attested that this fetus would not survive. A futile exercise the High Court said but it could happen again.
Finally, in addition to being an obstetrician, I am a specialist in fetal and maternal medicine. A significant part of this role is diagnosing fetal anomaly including anomaly that is not consistent with life outside the womb. This is a really difficult part of my job. You know when giving such devastating news that you change a family’s life irrevocably. In an instant.
In some cases women wish to continue their pregnancy knowing what will be but they tell me that whether or not their baby survives for a minute, an hour, a day or a week – this time is of infinite importance and they would not give it back.
Others however, find the prospect so horrific that to continue with the pregnancy would be too distressing.
Couples will choose to navigate these tragic circumstances in different ways. And to me that is understandable. For those who are unable to continue a pregnancy with no prospect of fetal survival, they find themselves forced to travel to a different jurisdiction to obtain termination of pregnancy. The constitution protects women who decide to travel but a termination in this country in this context would be a criminal offence. As an obstetrician I can only give limited practical support in this decision. They and their families must find this particularly cruel.
I have raised a number of difficult issues which I have encountered in my medical career.
No law will adequately address the reality of the ethical dilemmas generated by human reproduction. It is important that we are all aware of the inherent complexity of this whole subject and of the real risks that women face in clinically complicated pregnancies. If today’s proceedings advance this understanding – it is a good outcome.